WILLS POINT, TX – GFA World (Gospel for Asia) founded by K.P. Yohannan, has been the model for numerous charities like GFA World Canada, to help the poor and deprived worldwide, issued this Special Report update on Malaria making a comeback amid the worldwide impact of the COVID 19 Pandemic.
It’s a back-and-forth battle growing tougher in the face of COVID-19, with mosquitoes responsible for spreading the disease taking on the appearance of brass-helmeted warriors immune to nearly every device aimed in their direction. Malaria, humanity’s most deadly infectious disease, is making a comeback while our primary defense—net distribution—is being handicapped by the disruptions to normal life caused by the worldwide pandemic.
Insecticidal Nets a Mainstay, but Less Effective in Some Cases

That news appeared last summer in Nature Communications, which published research showing insecticide-treated mosquito nets—considered a mainstay in combating malaria—are not providing the protection they once did.1
According to another report in ScienceDaily, scientists say that’s cause for concern in tropical and subtropical countries. Long-Lasting Insecticidal Nets (LLINs) were credited with saving 6.8 million lives over a recent 15-year period.2
Dr. Stephen Carl, a malaria researcher in Australia, said LLINs add a community-level protective effect by significantly decreasing the mosquito population, which benefits even people not using nets. In Papua New Guinea, their introduction in 2006 led to a significant decline in cases, but between 2013–14 and 2016–17, the rate of infections rebounded from less than 1 percent to 7.1 percent.3
“[LLINs] are the only tools used at present in the national campaign against the mosquitoes that can carry malaria,” said study co-author Dr. Moses Laman.
While conclusions are still being formed on the news reported in Nature Communications, it appears diminished bioefficacy at the manufacturing level may be contributing to the problem of resurgence in malaria incidents.

Debating Treated Nets vs Untreated Nets
But not everyone agrees that treated nets are necessary. Research published just prior to the ScienceDaily report questioned if their cost makes the fight harder. One report in Malaria Journal said although more than 90 percent of the burden occurs in Africa, most prequalified nets approved by the World Health Organization (WHO) are manufactured elsewhere. The publication said many local manufacturers lack the capacity to produce insecticidal nets at a competitive scale and pricing.5
By relaxing conditions, it is conceivable that non-insecticidal but durable—and possibly biodegradable—nets could be readily manufactured locally, wrote author Fredros Okumu. While not aiming to discredit treated nets, he said he wanted to illustrate how a singular focus on insecticides can hinder innovation and sustainability.6
“The public health value of nets is increasingly driven by bite prevention, and decreasingly by lethality to mosquitoes,” Okumu said. “For context-appropriate solutions, it is necessary to acknowledge and evaluate the potential and cost-effectiveness of durable untreated nets across different settings.”
In his lengthy report, he also observed that developers should, instead of overemphasizing the need for new insecticides, ensure that bed nets are accessible, durable and properly used, even if non-insecticidal.
“New insecticides can then be developed for other forms of vector control,” Okumu said. “It has been demonstrated that resistant mosquitoes can survive up to 1,000-times the concentration of insecticides that kill susceptible populations. Such strongly resistant mosquitoes may naturally incur major survival and fitness costs in nature but are unlikely to be killed directly by insecticidal nets.”7

Fighting a Coronavirus that Hampers Bed Net Distribution
However one looks at the necessity of treated nets, distribution of any nets—treated or untreated—has been a cause for concern during the coronavirus outbreak.
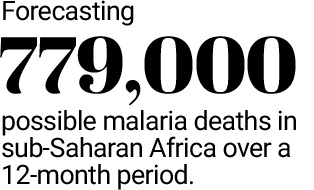
Writing in Nature Medicine, researchers forecast the possibility of 779,000 deaths in sub-Saharan Africa over a 12-month period, culminating in the summer of 2021.8 That compares to a WHO worst-case estimate of 769,000 malaria deaths this year, a mortality rate not seen in two decades.9
In the face of COVID-19, Okefu Oyale Okoko, deputy director of the National Malaria Elimination Programme in Nigeria, said it would still be important to ensure continuing deployment of vector control interventions to not only sustain gains in malaria elimination, but ensure against its resurgence.
According to a report in The (London) Telegraph, researchers concluded that treating children with fever as if they have malaria, even if not diagnosed with the disease, could save nearly 200,000 lives. And, of course, prompt distribution of bed nets could prevent hundreds of thousands of deaths.
When final statistics are available, researchers from the Imperial College of London predict if control programs were halted due to COVID-19, the number of cases during 2020 could double compared to 2019. In Nigeria alone, they said cutting treatment and delaying the distribution of bed nets could result in 81,000 additional deaths.

Typically distributed at community meetings, such gatherings to distribute bed nets faced interruptions over the last year because of event cancellations or poor attendance because of coronavirus fears.
Telegraph correspondent Anne Gulland wrote that researchers’ modeling found that provision of bed nets is critical since those treated with long-lasting insecticide have effects that continue for three years. More than half of the 47 countries most badly affected by the disease were due bed net distributions in 2020, with 228 million nets due to be handed out. That would have been the largest number ever.
James Whiting, executive director of Malaria No More UK, told the newspaper: “This important modelling is a reminder that efforts to end malaria sit on a knife edge. Protecting people against COVID-19 cannot be pursued in isolation. Governments must see maintaining efforts against malaria as a core part of pandemic preparedness or risk a catastrophic domino effect.”10
Soon after the Telegraph article, computer magnate turned philanthropist Bill Gates echoed the necessity of not allowing the pandemic to distract attention from the fight against mosquito-borne disease. The pesky insects are out infecting millions with a disease that kills a child every other minute daily, he wrote in his online blog.11
Gates—head of the Gates Foundation, a key non-governmental organization fighting malaria’s spread—said lockdowns and other regulations made it difficult for health workers to provide prevention and treatment across Africa. He said there were also interruptions to supplies of essential malaria tools like bed nets and anti-malaria medicines. Instrumental in reducing malaria deaths by more than half since 2000, he said interruption of these services could mean mortality levels not seen since the turn of the century.
“There is not a choice between saving lives from COVID-19 versus saving lives from malaria,” Gates wrote. “The world must enable these countries to do both. Health officials urgently need to step up to the challenge of controlling the pandemic while also making sure that malaria, as well as other diseases like HIV and tuberculosis, are not neglected.”12

“The world has changed in ways we could never imagine,” observed Dr. Pedro Alonso, director of the WHO’s Global Malaria Programme, in a letter to malaria partners six months after lockdowns began. “As COVID-19 began its rapid spread earlier this year from China to Italy, and beyond, alarm bells began ringing across the malaria community. After taking such a devastating toll on countries with robust health systems, how would malaria-endemic countries in Africa prevail? Among colleagues at WHO, there was deep concern that the coronavirus had the potential to upend years—perhaps decades—of progress in malaria control.”13
Progress Ebbs and Flows in the Fight to Beat Malaria
These recent developments place a heightened spotlight on World Malaria Day, observed on April 25. Fortunately, despite the high death toll and other troublesome signs lately, not all the news about malaria treatment is bad. There are gains amid the setbacks.

One positive example is Myanmar, where the annual malaria death toll of 3,800 a decade ago has decreased to approximately 170. The Global Fund to Fight AIDS, Tuberculosis and Malaria credits the efforts of 17,000 community volunteers who provide rapid testing and treatment, with serious cases referred to health facilities. Volunteers also educate the public through national antimalaria campaigns.14 Unfortunately, it’s unknown if the recent military coup in Myanmar will adversely impact the recent progress it’s achieved in the prevention of malaria.
News of another positive development appeared last October in Legion. About the same time the United States revealed a COVID-19 vaccine would be ready by the end of 2020, the Canadian magazine reported that a noted medical journal announced a new approach to fighting malaria.
Legion reported a clinical researcher for the U.S. National Institute of Allergy and Infectious Diseases has developed a vaccine for mosquito-borne diseases, based on mosquito spit. It causes the immune system to recognize mosquito saliva proteins and produce antibodies. The antibodies promote immunity by binding to pathogens to prevent them from damaging cells, plus coating pathogens and alerting other immune cells to attack and remove them.
“Those antibodies recognize the proteins the next time they’re encountered, sparking an immune response that goes into action to impair or prevent infection—and not just to malaria, it turns out,” wrote author Sharon Adams. “In animal studies, saliva vaccines impaired development of mosquito-borne Zika virus and sandfly-borne leishmaniasis.”15
In the first human trial of this vaccine in 2017, Adams said a strong immune response was observed among 49 volunteers, with only minor side effects. Next it will be tested on larger groups; if clinical trials continue to prove successful, the first effective malaria vaccine may be just around the corner.

In addition to this promising development, a European magazine carried a report from a healthcare company official saying there are antimalaria positives to be gained from the COVID-19 fight. Hogan Bassey, a Nigerian native who experienced several bouts with malaria as a child, noted that the pandemic highlighted system failings in global healthcare. He said if we are able to address those problems, the world will be better positioned to eradicate malaria and other diseases.
The chief innovation officer and founder of LivFul said his company is working with others—including nonprofits—to develop a repellent that it hopes will prove an efficient control tool. It has been working on a project in Ghana with a pharmaceutical company to improve one of the repellant’s ingredients, using LivFul’s technology to drive access.

“When we developed a revolutionary family-friendly insect repellent to halt the transmission of diseases like malaria and Dengue fever, we knew we could have a significant impact on insect-borne disease,” Bassey wrote in EPM Magazine. “If people in malaria-prone areas can purchase and use our repellent, these diseases can be stopped before they destroy lives, families, communities and industries.”16
Such a product won’t be the first tool developed. National Geographic recently reported hundreds of thousands of children across Kenya, Malawai and Ghana have been receiving the RTS,S vaccine, whose development has taken 35 years and cost hundreds of millions of dollars. While some African health professionals have asked if the expense and logistics of multiple vaccinations are worth it, the magazine said some Chinese scientists have been utilizing a new approach: preventing malaria from even occurring.
It goes back to 1972, when the Chinese discovered Artemisinin, a drug used to treat malaria. Now, scientists there believe Artemisinin Combination Therapies (ACTs) can be delivered to an entire community simultaneously, through Mass Drug Administrations. The goal is to reduce levels of the malaria parasite in human blood, so mosquitoes won’t contract it and spread it.
“The life cycle for a mosquito is 30 days,” explains Ethan Peng, senior manager in Kenya for the Chinese company New South, which manufactures ACTs. “So by mass medication, we can clear the source from all human beings (so) the mosquitoes cannot pick up on the malaria parasite again with their short lifespan.”17

Mosquito Nets Still the Leading Tool for Protection

When it comes to fighting malaria, the bed net still appears to be the leading tool. When COVID-19 hit in March 2020, WHO malaria scientist Pedro Alonso expected the biggest malaria disaster in 20 years after African countries temporarily suspended bed net campaigns.
That didn’t seem to be happening, the scientist said five months later. He credited lobbying by WHO’s Global Malaria Programme and its partners, which persuaded countries to resume their net distribution campaigns. Despite concerns over continuing COVID-19 problems, Alonso said, “We probably stopped the first big blow.”18
Among the many non-governmental organizations doing their part to distribute mosquito nets is Gospel for Asia (GFA).
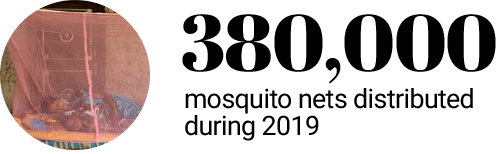 Since 2010, GFA has distributed more than 1.3 million nets to at-risk residents in mosquito-prone areas, including 380,000 in 2019 (many are treated with insecticide, with availability depending on local conditions).
Since 2010, GFA has distributed more than 1.3 million nets to at-risk residents in mosquito-prone areas, including 380,000 in 2019 (many are treated with insecticide, with availability depending on local conditions).
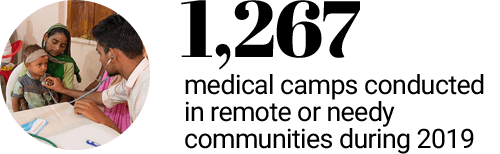 These efforts are augmented by distribution of malaria pills at GFA’s medical camps. In 2019 the organization hosted nearly 1,300 camps, which are free to attendees.
These efforts are augmented by distribution of malaria pills at GFA’s medical camps. In 2019 the organization hosted nearly 1,300 camps, which are free to attendees.
The difference net distributions make can be seen in the stories of people like Baharupa, a 55-year-old farmer and father of three who felt pressured to drink alcohol at many village-wide events. Not only did he often wind up drunk, he developed an addiction. That all changed after Satyam, a Gospel for Asia (GFA) worker, organized a distribution of 4,000 nets.

“Who can give us mosquito nets without money?” Baharupa wondered. “This shows [the believers’] love towards us.”19This experience so touched Baharupa that it began a transformation in his life.
Another story of relief involves a 71-year-old widow whose husband had died more than a decade prior. With four daughters all married, Bhranti spent evenings alone, worried about the tattered net providing her only protection from mosquitoes. She received a new net through a distribution organized by a Gospel for Asia (GFA) worker.
“I am so grateful to the [GFA workers] for their love and care and for providing a mosquito net,” Bhranti says. “Now I do not need to worry about buying a mosquito net as I have been provided a new one.”20
Even amid the problems COVID-19 has caused in poorer parts of the world, GFA’s supporters have been able to help local workers in the field save lives and prevent more tragedies during the pandemic, says GFA’s founder, Dr. K.P. Yohannan.

GFA World Founder
“Without proper prevention or treatment, the consequences of a simple mosquito bite are very serious in many places of the world,” Yohannan says. “But for just $10, we can protect numerous lives, one net at a time.”
What can we do about mosquito-driven scourges? »
One simple way to fight mosquito-borne diseases like malaria, is to consider giving a needy family a simple Mosquito Net. For only $10, Gospel for Asia’s field partners can distribute one of these effective nets to an at-risk family in Asia and provide them with safety from insects during the day and at night.
About GFA World
GFA World (formerly known as Gospel for Asia) is a leading faith-based global mission agency, helping national workers bring vital assistance and spiritual hope to millions across the world, especially in Asia and Africa, and sharing the love of God. In GFA World’s latest yearly report, this included thousands of community development projects that benefit downtrodden families and their children, free medical camps conducted in more than 1,200 villages and remote communities, over 4,800 clean water wells drilled, over 12,000 water filters installed, income-generating Christmas gifts for more than 260,000 needy families, and teaching providing hope and encouragement available in 110 languages in 14 nations through radio ministry. In the years ahead, GFA World expects to launch programs in numerous African nations, starting with compassion projects in Rwanda. For all the latest news, visit our Press Room at https://press.gfa.org/news.
Read more news on GFA World, Malaria, Mosquito Nets and the COVID 19 Pandemic.
Learn more by reading this Special Report from Gospel for Asia: Winning the Ancient Conflict Between Man and Mosquito — Know Your Enemy or Succumb to Vector-borne Diseases
KP Yohannan has issued two statements about the COVID-19 situation found here and here.
Read what 25 Christian Leaders are affirming about Gospel for Asia.
This Special Report originally appeared on gfa.org.





