WILLS POINT, TX – Gospel for Asia (GFA World and affiliates like Gospel for Asia Canada) founded by KP Yohannan, issued a Special Report on how the alarming increase of mosquito-blamed cases in U.S. in may awaken Westerners to the “deadly scourge” of malaria that still claims thousands of lives worldwide.
Because the deaths came in ones and twos, the mid-summer and early fall 2019 headlines were more local than national in scope. They told of a 70-year-old man in Massachusetts—one of 10 people infected in the state—dying from Eastern equine encephalitis (EEE)s, a virus transmitted through a mosquito bite; two deaths in Connecticut, where officials identified EEE-carrying mosquitoes in a dozen municipalities; and a 68-year-old man in Ohio who died from mosquito-linked West Nile virus.

Before the year ended, more than a dozen fatalities had been recorded. As of mid-November, the Centers for Disease Control reported three dozen cases of EEE in 2019, the highest in 60 years.[1] The annual average for the previous decade: just seven.
Granted, a relative handful of tragic fatalities from EEE doesn’t compare to thousands of deaths attributed each year to malaria, which still vexes health officials centuries after its discovery. Still, this five-fold increase in EEE cases may help sensitize Americans to the scourge of mosquito-borne health dangers. Such an awakening is especially timely with the observance of World Malaria Day on April 25, which draws attention to the 400,000 lives per year lost to this deadly disease.
In fact, while the total number of confirmed COVID-19 cases worldwide (on the date of this report) currently stands at 2.5 million and rising, each year there are more than 200 million reported cases of malaria, mostly in sub-Saharan Africa and South Asia.
A previous special report on this topic, entitled “Fighting Malaria – A Chilling Disease,” details how mosquito netting and malaria prevention are being used to combat this parasitic genius. This update unfolds the ongoing efforts of the global community to combat mosquito-borne scourges, including malaria, even among developing nations.
Despite advances in recent years, malaria remains a leading cause of death globally.
There was a mixture of good and bad news in the report.
Despite advances in recent years, malaria remains a leading cause of death globally.
There was a mixture of good and bad news in the report.
Advancements in the Fight
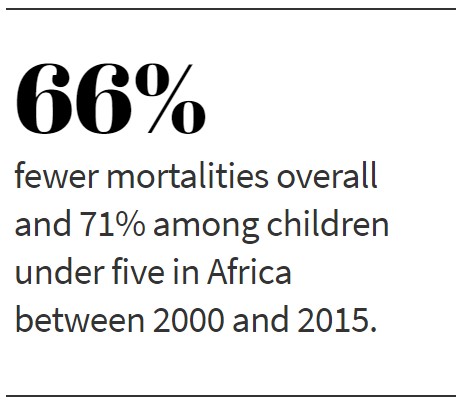
Thanks to a consortium of governments, foundations and non-governmental organizations, there have been advancements in treatment. In 2015 the WHO announced the global incidence of malaria had finally slowed: Between 2000 and 2015, mortality rates in Africa fell by 66 percent overall and 71 percent among children under 5, the most vulnerable victims.[3]
 “The last decade has seen a significant transition in the ways that countries are responding to malaria,” Dr. David Reddy, CEO of the partnership, Medicines for Malaria Venture, said in a 2015 interview. “Significant new international resources (including Global Fund and President’s Malaria Initiative) have been better mobilized in the last 10–15 years to support programmatic strengthening and introduce greatly improved tools to prevent and treat malaria.”[4]
“The last decade has seen a significant transition in the ways that countries are responding to malaria,” Dr. David Reddy, CEO of the partnership, Medicines for Malaria Venture, said in a 2015 interview. “Significant new international resources (including Global Fund and President’s Malaria Initiative) have been better mobilized in the last 10–15 years to support programmatic strengthening and introduce greatly improved tools to prevent and treat malaria.”[4]
In his foreword to the WHO’s 2019 report, Director-General Dr. Tedros Adhanom Ghebreysus noted that at least 10 countries are on track to reach the 2020 elimination milestone set in its long-term global strategy. In 2015, he said all those countries were malaria endemic, but now have either achieved zero indigenous cases or are nearing that goal.

More resources are appearing too. Just before the release of the WHO report, the board of the Geneva-based Global Fund to Fight AIDS, Tuberculosis and Malaria approved increased funding for investments over a three-year period (starting in 2020) to fight these epidemics. The investments total more than $12.9 billion U.S. as of March 2020.
Medical advances are occurring as well. In September of 2019, a paper in Science Translation Medicine described how redesigning molecules first designed to treat a skin disease (psoriasis) could lead to an effective new drug. An international team of researchers described modifying a class of molecules called pantothenamides to increase their stability in humans. In brief, the new compounds stop the malaria parasite from replicating in infected people and are effective against parasites resistant to current drugs.[5]
One of the paper’s authors, Penn State University professor Manuel Llinás, said while pantothenamides are potent against parasites, they become unstable within biological fluids because an enzyme clips them apart before they can act. Changing a chemical bond prevents this from happening.
“By also preventing the transmission of malaria parasites from infected people into mosquitoes, these pantothenamides can reduce the chances that mosquitoes will be infectious to others,” Llinás said. “It is currently widely accepted that next-generation antimalarial drugs must target the parasite at multiple stages to both cure the disease in an infected individual and prevent its spread to others.”
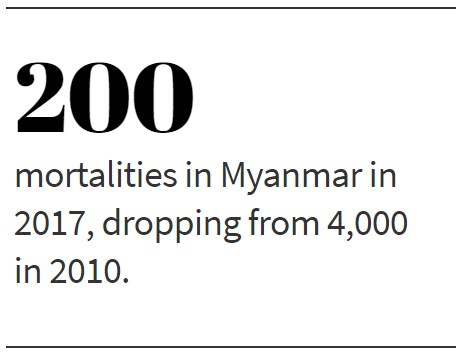 This news came on the heels of a story by Joshua Carroll in The Guardian newspaper about Myanmar becoming an example in the fight against malaria. It chronicled how thousands of volunteers received training and supplies from donors after political reforms opened the door for a flood of aid.
This news came on the heels of a story by Joshua Carroll in The Guardian newspaper about Myanmar becoming an example in the fight against malaria. It chronicled how thousands of volunteers received training and supplies from donors after political reforms opened the door for a flood of aid.
These efforts helped save thousands of lives and turned Myanmar into a leader in the battle to eliminate the disease. Nationwide in 2010 nearly 4,000 people died from malaria, but in 2017 that number dropped to 200.
“Dr. Patricia Graves, a leading specialist on the transmission and control of malaria, is confident Myanmar is on track to be malaria-free by 2030,” Carroll wrote. “The country’s success with village-based health workers ‘is a huge thing that other countries can learn from,’ she says.”[6]

Rising to the Challenge
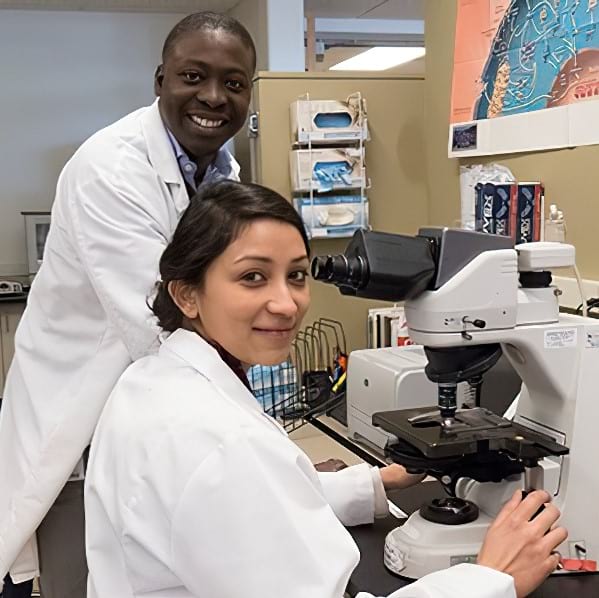
One of the ironies in the fight against malaria is that past victims are combating it, including people like Dr. Nana Minkah, a scientist at the Kappa Lab at Seattle Children’s Hospital. Growing up in the sub-Saharan nation of Ghana, he contracted the disease multiple times. Among his memories are bouts when he spent more than a week in bed with pain and chills so bad he visibly shivered.
In 2015, after earning a Ph.D. in molecular genetics and biology, Dr. Minkah joined the Kappa Lab. Even though he didn’t have experience in parasitology, he wanted to work on malaria, especially since it still plagues his homeland.
One of the ways the lab hopes to pioneer new methods of preventing malaria is with genetically engineered vaccines. In March of 2019, it successfully completed a vaccine with a first-generation strain of the most lethal parasite. Such vaccines rely on a basic principle: to give the immune system an advantage over a pathogen by teaching it to recognize the invader before the infection occurs.
“I wanted to do work that has clinical implications with the potential to save the lives of people who look like me,” Dr. Minkah said. “What we are trying to do is a tall order. We are trying to develop a product that will create unnatural immunity.”[7]
Despite such inspiring stories, challenges still exist. For example, while malaria was eliminated in the U.S. in 1951, the country still has Anopheles mosquitoes that can bite an infected person and transmit to others.

During last summer’s EEE outbreak, health officials in five southwest Michigan counties warned of a “critical risk” of the virus in 35 communities, with another 40 at high risk. Dr. Brian Chow, a doctor of infectious diseases at Tufts Medical Center, said 2019 seemed to be much more severe than in years past. “It is a concern,” Chow said.[8]
Such situations point to the vigilance needed for the fight. A 2019 article in the Scientific American pointed out how, over time, drug treatment of the disease lose their effectiveness as parasites grow resistant to it. For example, in the 1990s, chloroquine was of first-line importance in Africa. By the early 2000s, that drug was replaced by sulfadoxine/primethamine and later ACTs (for Artemisinin Combination Therapy). Each time, resistance developed.
“While mutation in this gene has occurred in Southeast Asia and is spreading around the region, there are fears it will spread to Africa, like it did for the drugs before it,” wrote Ify Aniebo, a research scientist and fellow at Harvard’s school of public health. “The more drugs we use to treat malaria parasites, the more resistant they become due to selective pressure.”[9]
Ironically, even as parasites adapt to resist technology, one of the most effective methods to combat malaria is rather old-fashioned: mosquito nets. A study of Africa released in the spring of 2019 found that the single-most important factor to a 15-year decline in malaria fatalities—from 840,000 deaths in 2000 to 440,000 in 2015—was increased distribution of insecticide-treated bed nets. The authors of the study estimate they were responsible for averting 451 million cases during that 15-year period.[10]
Joining the Fight
This study highlights the importance of one group’s primary methods of fighting the disease in South Asia: distributing mosquito nets free of charge to vulnerable families. Workers supported by Gospel for Asia (GFA) distributed 360,000 nets in 2018.

“As GFA combats these mosquitoes and the deadly disease they carry, we’re seeking to minimize the risk of children being infected,” founder K.P. Yohannan says in a 2019 press release for World Malaria Day. “It’s part of our commitment to the remote communities and one way to express God’s love for them. Many villagers in remote areas can’t afford to buy mosquito nets or preventive medications. This is why our efforts are so critical.”
Distribution of nets is only one aspect of multi-faceted efforts by GFA in these areas. The ministry also supports workers who hold free health seminars, distribute vitamins and educate villagers about hygienic routines to reduce the potential for disease and infection.
Such efforts create heart-rending anecdotes, like that of Pastor Ronsher, who serves in an area with high transmission rates. There, impoverished farmers and daily wage laborers struggle to secure proper medical care and hygiene; among their numbers is a couple named Bahman and Salli, whose daughter had been paralyzed for three years. After Pastor Ronsher gave them a net, he visited them for several weeks to teach them how to use it and offer encouragement.
“You helped us by providing a piece of mosquito net in our lives, though you never knew us before,” Bahman said. “Many knew about our problems, but except [for] you, none of them showed their kindness toward us. We are touched with your love.”
Such love may be needed for those living in the U.S. as well. In addition to the increased rate of Eastern Equine Encephalitis cases last year, one malaria researcher at the University of Maryland’s medical school recently warned of limited access to an intravenously-administered drug. The IV treatments are needed for the more serious cases of mosquito-linked diseases in America.

“Severe malaria is a medical emergency that requires immediate treatment with IV medication to reduce the risk of death,” says Dr. Mark Travassos, a pediatric infectious diseases specialist who cited a 2015 Centers for Disease Control and Prevention report showing 1,500 malaria cases in the U.S., of which 259 needed IV treatment.[11]
Dr. Travassos says while oral treatments for malaria are available, in the U.S. these are often not effective in more serious cases: “Severe malaria patients can have brain involvement or repeated vomiting and may not tolerate oral medication, placing them at high risk for complications.”
As his University of Maryland associate, Professor Kathleen Neuzil, puts it, “Malaria is a leading killer worldwide, impacting millions of people each year. While we continue to work on developing vaccines and other treatments, it is critical that patients everywhere have access to the regimens needed to combat this disease.”
That means patients in places as poor as South Asia and as affluent as the U.S.
What can we do about mosquito-driven scourges?
One simple way to fight mosquito-borne diseases like malaria, is to consider giving a needy family a simple Mosquito Net. For only $10, Gospel for Asia’s field partners can distribute one of these effective nets to an at-risk family in Asia and provide them with safety from insects during the day and at night.
Read more news on Malaria and Gospel for Asia on MissionsBox News.
This Special Report originally appeared on gfa.org.
Read another Special Report from Gospel for Asia on Fighting Malaria – A Chilling Disease: Mosquito Netting and Malaria Prevention Combat a Parasitic Genius.
Learn more by reading this special report from Gospel for Asia: It Takes Only One Mosquito – to lead to remarkable truths about faith-based organizations and world health.





